Postop care of your joint replacement
Discharge instructions for hip replacement / hip resurfacing (posterior approach)
- Do not flex the hip over 90 degrees and do not cross your knees.
- Please, take with you the elastic stockings that were provided to you in the hospital, or get a pair of support socks in a medical supply pharmacy. Have someone put on your elastic stockings in the morning and have them removed at night before going to bed. Use large, comfortable shoes so you can easily put them on and take them off, without having to reach your foot. You also need assistance to put on your shoes, and cut your toenails; the flexion required to reach your foot may cause the hip to dislocate in the early postoperative period.
- Sit in a high armchair. The height should be approximately 25” if you are 6’ or taller, 22” if you are about 5½’ and 20” if you are 5’ or less. Use your hands to assist yourself in sitting and rising from the high armchair. Use a high toilet seat. Sitting in a low seat may dislocate the hip before it heals.
- At night, sleep with a pillow between your thighs and knees; you may turn in bed as long as a pillow is between your knees. You can lie on the operated side if it does not hurt you.
- You cannot drive a car for the first five weeks after surgery. You could be a passenger, provided you are very careful getting in and out of the car. Place the seat high, back and recline the back-seat backwards.
- You can take showers before your staples/stiches are removed, providws that the incision is completely covered by a water-proof dressing. I recommend: “3M Tegaderm 6x8 inch dressing” that can be purchased in your local pharmacy or on the internet. The incision does not need to be covered when taking a shower; after that staples/stitches are removed. Get into the shower as instructed by the physical therapist.
- PHYSICAL THERAPY: Follow the instructions given to you by the physical therapist at the hospital, regarding the use of a cane, crutches or walker, as well as the amount of weight that you were instructed to put on the operated leg. Continue the exercises as instructed and as tolerated. If your hip hurts, don’t do them until the pain subsides. The exercise that involves flexion and extension of your ankles and feet is essential and you should do it several times a day. It will prevent the formation of clots in your veins. If you were discharged home, you will see a visiting physical therapist a few times per week. Please make sure that his/her instructions do not contradict the ones provided by me. After graduating from your home physical therapy program, you may continue practicing the exercises at home or start outpatient physical therapy. A script is provided with this package. Please make sure that your physical therapist complies with my discharge instructions to avoid injury or complications.
- ANTICOAGULATION: Depending on the type of surgery and your past medical history, I will prescribe a mild (aspirin) or a potent blood thinner after surgery (Coumadin - Xarelto):
- If you are not on aspirin, continue taking Ascriptin (Aspirin) 325mg, one after breakfast and one after dinner for another two weeks. Thereafter take only one after breakfast until you complete 6 weeks of treatment after the operation.
- If you are on warfarin/Coumadin, the daily dose is dictated by the internist who cleared you for surgery at HSS. You need periodic blood tests to decide the daily dose of warfarin/Coumadin. At home, visiting nurses will order the tests. Make sure the results are transmitted to your internist who will advise the adequate daily dose. This is paramount to prevent bleeding or inadequate anticoagulation.
- If you are on Xarelto, continue taking 10mg, once daily for the first five postoperative weeks.
- Some hip pain and swelling that could extend down to your leg is not unusual during the first few weeks after surgery, and it should ease as time goes by. Your walking distance and level of activities can progressively increase according to how your hip feels.
- PAIN MEDICATION: Good pain control is important for a prompt recovery. You will probably need prescription pain medication during the first weeks after surgery. You will leave the hospital with the necessary prescriptions. If you need refills or a change in the type of pain medication, please plan ahead and let my office know at least 7 days in advance.
- You may have swelling in the hip area that could extend down to the thigh and leg. You may also have black and blue bruising. It will subside in a few weeks, particularly if you follow the enclosed Swelling Instructions.
- Read carefully the manual you received at the preoperative class Your Pathway to Recovery following Total Hip Replacement. It will provide useful information.
The above is intended as a general guide during the first five to eight weeks after total hip replacement. On your next visit, and depending upon your progress, activities are usually increased and restrictions decreased. Additional instructions and educational videos can be obtained at www.agdvmd.com
If you cannot keep this appointment, please call to re-schedule at least 72 hours in advance.
Discharge instructions for hip replacement (anterior approach)
- Do not rotate your leg out while bringing it back behind you.
- Please, take with you the elastic stockings that were provided to you in the hospital, or get a pair of support socks in a medical supply pharmacy. Have someone put on your elastic stockings in the morning and have them removed at night before going to bed. Use large, comfortable shoes so you can easily put them on and take them off, without having to reach your foot. You also need assistance to put on your shoes, and cut your toenails; the flexion required to reach your foot may cause the hip to dislocate in the early postoperative period.
- During the first weeks, you may find it beneficial to sit in a high armchair, and to use a high toilet seat.
- At night, sleep with a pillow between your thighs and knees; you may turn in bed as long as a pillow is between your knees. You can lie on the operated side if it does not hurt you.
- You cannot drive a car for the first four weeks after surgery. You could be a passenger, provided you are very careful getting in and out of the car. Place the seat high, back and recline the back-seat backwards.
- The staples/stitches should be removed 12 to 15 days after surgery. Before you leave the hospital, ask the nurse for a staple removal kit. The staples can be removed in the rehabilitation center or by a local nurse or doctor. Otherwise, please call my office for an appointment and I will be glad to remove them for you.
- You can take showers before your staples/stiches are removed provided that the incision is completely covered by a water-proof dressing. I recommend: “3M Tegaderm 6x8 inch Dressing” that can be purchased in your local pharmacy or on the internet. The incision does not need to be covered while shower; after that staples/stitches have been removed. Get into the shower as instructed by the physical therapist.
- PHYSICAL THERAPY: Follow the instructions given to you by the physical therapist at the hospital, regarding the use of a cane, crutches or walker, as well as the amount of weight that you were instructed to put on the operated leg. Continue the exercises as instructed and as tolerated. If your hip hurts, don’t do them until the pain subsides. The exercise that involves flexion and extension of your ankles and feet is essential and you should do it several times a day. It will prevent the formation of clots in your veins. If you were discharged home, you will see a visiting physical therapist a few times per week. Please make sure that his/her instructions do not contradict the ones provided by me. After graduating from your home physical therapy program, you may continue practicing the exercises at home or start outpatient physical therapy. A script is provided with this package. Please make sure that your physical therapist complies with my discharge instructions to avoid injury or complications.
- ANTICOAGULATION: Depending on the type of surgery and your past medical history, I will prescribe a mild (aspirin) or a potent blood thinner (Coumadin or Xarelto) after surgery:
- If you are not on aspirin, continue taking Ascriptin (Aspirin) 325mg, one after breakfast and one after dinner for another two weeks. Thereafter take only one after breakfast until you complete 6 weeks of treatment after the operation.
- If you are on warfarin/Coumadin, the daily dose is dictated by the internist who cleared you for surgery at HSS. You need periodic blood tests to decide the daily dose of warfarin/Coumadin. At home, visiting nurses will order the tests. Make sure the results are transmitted to your internist who will advise the adequate daily dose. This is paramount to prevent bleeding or inadequate anticoagulation.
- If you are on Xarelto, continue taking 10mg, once daily for the first five postoperative weeks.
- Some hip pain and swelling that could extend down to your leg is not unusual during the first few weeks after surgery, and it should ease as time goes by. Your walking distance and level of activities can progressively increase according to how your hip feels.
- PAIN MEDICATION Good pain control is important for a prompt recovery. You will probably need prescription pain medication during the first weeks after surgery. You will leave the hospital with the necessary prescriptions. If you need refills or a change in the type of pain medication, please plan ahead and let my office know at least 7 days in advance.
- You may have swelling in the hip area that could extend down to the thigh and leg. You may also have black and blue bruising. It will subside in a few weeks, particularly if you follow the enclosed Swelling Instructions.
- Read carefully the manual you received at the preoperative class Your Pathway to Recovery following Total Hip Replacement. It will provide useful information.
The above is intended as a general guide during the first five to eight weeks after total hip replacement. On your next visit, and depending upon your progress, activities are usually increased and restrictions decreased. Additional instructions and educational videos can be obtained at www.agdvmd.com
If you cannot keep this appointment, please call to re-schedule at least 72 hours in advance.
Discharge instructions for total or partial knee replacement
- Please, take with you the elastic stockings that were provided to you in the hospital, or get a pair of support socks in a medical supply pharmacy. Have someone put on your elastic stockings in the morning and have them removed at night before going to bed. Use large, comfortable shoes so you can easily put them on and take them off, without having to reach your foot.
- PHYSICAL THERAPY: Follow the instructions given to you by the physical therapist at the hospital, regarding the use of a cane, crutches or walker, as well as the amount of weight that you were instructed to put on the operated leg. Do the exercises instructed by me and by your physical therapist to achieve the best possible result. The most important ones are depicted below. During the first weeks, you will gain most of the mobility of your knee. You must exercise consistently. You might feel discomfort or pain while exercising. If the pain is severe, stop and ice your knee. Take the pain medication one hour before exercising and ice your knee afterwards. The exercise that involves flexion and extension of your ankles and feet should be done as much as possible as it will prevent the formation of clots in your veins.
- IMPORTANT NOTICE ABOUT PAIN MEDICATION AFTER SURGERY: Good pain control is important for a prompt recovery. You will need prescription pain medication during the first months after surgery. You will leave the hospital with the necessary prescriptions. Please take the pain medication as prescribed to you in the hospital. If you need refills or a change in the type of pain medication, please plan ahead and let my office know at least 7 days in advance.
- Apply ice to your knee intermittently. You should feel a pleasant cool sensation, not a burning sensation by the ice. Take the pain medication as instructed. A painless knee will rehabilitate better and faster than a painful one.
- It will be more comfortable to sit in a high armchair, particularly one with armrest. Use your hands to assist youself in sitting and rising from the chair. Use a high toilet seat.
- If you had a right knee replacement or bilateral knee replacements, you cannot drive a car for the first five weeks after surgery. If you had a left knee replacement and you have a car with automatic transmission, you can drive as soon as you feel comfortable sitting on the driver’s seat. YOU SHOULD NOT DRIVE if you are under the effect of the potent pain medication prescribed after surgery. You could be a passenger, provided you are very careful getting in and out of the car. Place the seat high, back and recline the back-seat backwards.
- Do not place towels or pillows under your knee. While in bed, keep your knee straight with the foot pointing to the ceiling, and not rotated out. Exercise #1 should be performed frequently to prevent your knee from healing bent.
- IMPORTANT NOTICE ABOUT ANTICOAGULATION AFTER SURGERY: Depending on the type of surgery and your past medical history, I will prescribe a mild (aspirin) or a potent blood thinner after surgery (Coumadin-Xarelto):
- If you are on aspirin, continue taking Ascriptin (Aspirin) 325mgs, one after breakfast and one after dinner for another two weeks. Thereafter take only one after breakfast until you complete 6 weeks of treatment after the operation.
- If you are on Coumadin, the daily dose is dictated by the internist/rheumatologist/cardiologist that cleared you for surgery in HSS. You need periodic blood tests to determine the daily dose of Coumadin. If you are at home, visiting nurses will order the tests. Make sure the results are transmitted to your internist who will advise the adequate daily dose. This is paramount to prevent severe bleeding or inadequate anticoagulation.
- If you are on Xarelto, continue taking 10mg, once daily for the first three postoperative weeks.
- Some knee pain and swelling that could extend down to your leg is not unusual during the first few weeks after surgery, and it should ease as time goes by. Your level of activities can progressively increase as long as you have no knee pain. Your walking distance and level of activities can progressively increase according to how your knee feels.
- You may have swelling in the knee area that could extend to the thigh and leg. You may also have black and blue bruising. It will subside in a few weeks, particularly if you follow the Swelling Instructions in this package.
- The staples should be removed 12 to 15 days after surgery. Ask the nurse for a staple removal kit before you leave the hospital. The staples can be removed in the rehabilitation center or by a local nurse or doctor. Otherwise, please call my office for an appointment and I will be glad to remove them for you.
- You can take showers before your staples/stiches are removed providing that the incision is completely covered by a water-proof dressing. I recommend: “3M Tegaderm 6x8 inch dressing” that can be purchased in your local pharmacy or in the internet, or a plastic bag carefully taped around your thigh. The incision does not need to be covered when showering after that staples/stitches have been removed. Get into the shower as instructed by the physical therapist.
- If you had a total knee replacement, read carefully the manual you received at the preoperative class “Your Pathway to Recovery following Knee Replacement”. It will provide useful information.

If you were discharged home, you will see a visiting physical therapist a few times per week. Please make sure that his/her instructions do not contradict the ones provided by me. After graduating from your home physical therapy program, you may start outpatient physical therapy. A script is provided with this package.
The above is intended as a general guide during the first five to eight weeks after knee replacement surgery. On your next visit, and depending upon your progress, activities are usually increased and restrictions decreased. Additional instructions and educational videos can be obtained at www.agdvmd.com
If you cannot keep this appointment, please call to re-schedule at least 72 hours in advance.
Discharge instructions for knee arthroscopy
Coming soon
Discharge instructions for knee cartilage transplant
Coming soon
Leg swelling instructions
Swelling of your operated area, extending to the thigh and leg is not unusual after surgery, including areas of “black and blue”. These instructions should help to overcome the swelling:
- Use elastic stockings during the day. Have someone put the stockings on when you get up from bed in the morning and have them removed at night. If you were not provided with the stockings at the hospital, please use a pair of support socks that can be bought in a medical supply store, department store or online (footsmart.com – Moderate support microfiber socks).
- Exercise your toes, feet, and ankles up and down (“pump”) for a few minutes every hour. This exercise should be done vigorously and not too fast. Count to three between extension and flexion of your ankles and toes.

- Have someone massage your leg upwards from the foot to the knee, mobilizing the fluid within the tissues upwards.
- Avoid sitting with your legs hanging down. Sit with the legs partially elevated. Again, exercise your toes, feet, and ankles frequently up and down, while you are sitting.
- Do not stand for long periods of time. If you have to, stand repeatedly on your tiptoes.
- After lunch lay down for an hour or so and keep on “pumping” toes, feet and ankles.
- If the swelling persists in both legs consult your internist, as you may need a diuretic, a drug to reduce your body water content.
- Once the swelling is gone, remove the elastic stockings in the late afternoon. If the legs do not swell, remove the stockings a few hours earlier on the next day, and so on. After a few days, you will not need them any longer.
- If the swelling persists despite following these instructions, particularly if the leg is swollen when you wake up in the morning, please call my office or the office of your HSS internist.
Additional information, instructions and educational videos can be obtained at www.agdvmd.com
Swelling of your operated area, extending to the thigh and leg is not unusual after surgery, including areas of “black and blue”. These instructions should help to overcome the swelling:
If you cannot keep this appointment, please call to re-schedule at least 72 hours in advance.
Insomnia instructions
Your recent surgery may transiently affect your sleeping habits. Do not worry! Over 100 million Americans are estimated to have occasional sleep problems, and about one in six has chronic insomnia.
To return to your normal sleeping habits and because of the negative side effects from sleep medications, we recommend you follow these guidelines:
Do not take naps during the day. Reduce your intake of fluids after 8:00 p.m. to avoid waking up because of a full bladder. Refrain from evening use of alcohol, caffeine and nicotine. As your operated hip recovers, increase daily physical exercise but refrain from exercising within 3 hours of bedtime. Delay bedtime by about 1 hour. Establish a regular wind-down period 1 or 2 hours prior to bedtime. Do not spend more than 7 or 8 hours in bed.
Use the bedroom for sleep and relaxing activities only. Make sure the temperature of your bedroom is comfortable. In general, a cooler room facilitates sleep. Go to bed when drowsy. Read or watch television until very drowsy, then turn the lights off and go to sleep. If not asleep within half an hour, do not try to sleep; instead, engage in a relaxing activity (e.g. reading) and do not attempt to sleep until drowsy again. Repeat this as often as necessary.
Get up at about the same time every day (including weekends), even if you have had a poor night’s sleep.
If your sleep does not improve after a few months an evaluation from a sleep clinic may be indicated.
Additional information and educational videos can be obtained at www.agdvmd.com
5 to 8 weeks instructions after hip replacement / hip resurfacing (posterior approach)
You have completed the most crucial postoperative period. From now on you can increase your activities progressively and as tolerated, provided your hip does not hurt.
- You can discontinue the added height of your armchair, bed and toilet seat. You may find to be more comfortable sitting in higher seats with arm rests.
- You do not need the pillow between your legs at night, and you can turn in bed to either side, even without the pillow. You can sleep on your stomach.
- If your legs are not swollen in the evening, you can give up the elastic stockings.
- If you had a standard total hip replacement, as soon as you feel confident and can walk without pain or limp, you can give up the cane. If you had a revision or other type of operation, I will indicate how much weight you should put on your hip.
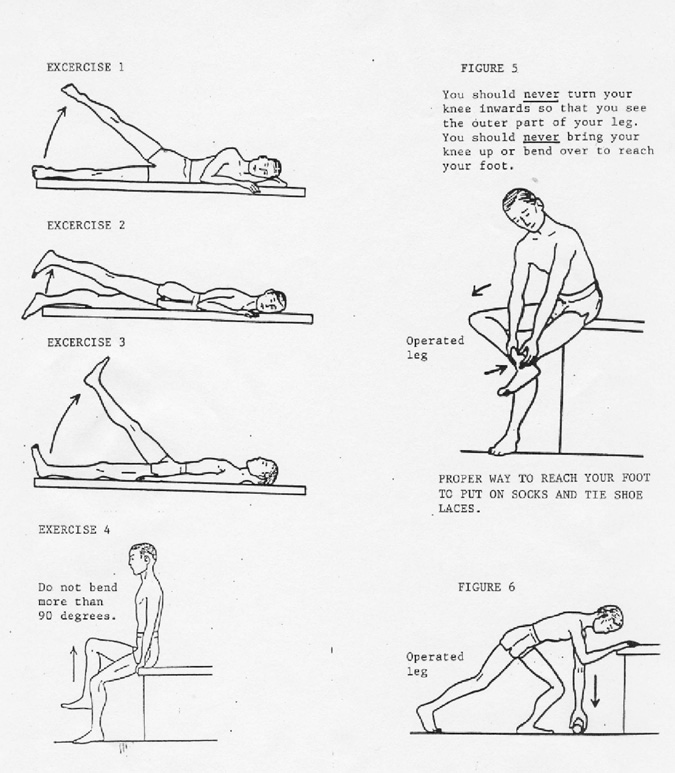
- In addition to your previous exercises, start the exercises shown on the back of this sheet (Exercises 1 to 4 on the next page). Increase the number of repetitions as tolerated. If it hurts don’t do them until the pain subsides. You can also do exercises 1, 2 and 3 standing, which requires less effort.
- You can now try to reach your foot. While reaching, bring the knee outwards and the foot inwards as shown in Figure 5. This is a long-term goal and it may take a few more weeks for you to be able to reach the foot. While reaching your foot, you should always see the inner part of your thigh and leg, and not the outer part of your leg. This precaution is for life.
- To pick up objects from the floor, lean on a piece of furniture and do it as shown in Figure 6.
- Have showers rather than baths. Place a handle on the shower wall and a footstool outside and inside to help you in and out.
- You may now drive a car.
- If you are experiencing problems, please return to see me four months after surgery for an examination of your operated hip. If you experience no problems, please see me 1 year after surgery with new X-rays, instead.
- Long term care: You should have periodic examinations and x-rays of your hip replacement. I will discuss with you the frequency of such visits based on your age and activity level. Follow us on Facebook, Twitter and Instagram (@NYHipKnee ) for periodic updates on conditions that may affect your hip replacement as well as updates on how to make it last longer.
For additional information, instructions and educational videos please visit www.agdvmd.com
5 to 8 weeks instructions after hip replacement (anterior approach)
You have completed the most crucial postoperative period. From now on you can increase your activities progressively and as tolerated, provided your hip does not hurt.
- You can discontinue the added height of your armchair, bed and toilet seat, if you are still using them. You may find to be more comfortable sitting in higher seats with arm rests.
- You can turn in bed to either side. You can sleep on your stomach.
- If your legs are not swollen in the evening, you can give up the elastic stockings.
- If you had a standard total hip replacement, as soon as you feel confident and can walk without pain or limp, you can give up the cane. If you had a revision or other type of operation, I will indicate today how much weight you should put on your hip today.
- You can now try to reach your foot to put on a pair of socks and tie shoelaces.
- Have showers rather than baths. Place a handle on the shower wall and a footstool outside and inside to help you in and out.
- You may drive a car.
- If you are experiencing problems, please return to see me four months after surgery for an examination of your operated hip. If you experience no problems, please see me 1 year after surgery with new X-rays, instead.
- Long term care: You should have periodic examinations and x-rays of your hip replacement. I will discuss with you the frequency of such visits based on your age and activity level. Follow us on Facebook, Twitter and Instagram (@NYHipKnee) for periodic updates on conditions that may affect your hip replacement as well as updates on how to make it last longer.
For additional information, instructions and educational videos please visit www.agdvmd.com
5 to 8 weeks instructions after partial or total knee replacement
You have completed the most critical postoperative period. From now on you can increase your activities progressively and as tolerated, provided your knee does not hurt.
- You can discontinue the added height of your armchair, bed and toilet seat.
- You can turn in bed to either side, and you can sleep on your stomach.
- If your legs are not swollen in the evening, you can give up the elastic stockings.
- If you had a standard total or partial knee replacement, you can give up the cane as soon as you feel confident and can walk without pain or limp. If you had a revision or other type of operation, I will tell you how much weight you should put on your knee.
- You should continue with your previous exercises, and those depicted below. You should do them several times a day. The window of opportunity for you to gain range of motion after surgery is limited. Therefore, I strongly encourage you to perform these exercises frequently, enthusiastically and vigorously to achieve the best possible result.

- IMPORTANT NOTICE ABOUT PAIN MEDICATION: Good pain control is important for a prompt recovery. You may still experience pain in the operated area and may need prescription pain medication for the next weeks. If you need refills or a change in the type of pain medication, please plan ahead and let my office know at least 7 days in advance. If a prescription for pain medication needs to be mailed to your pharmacy, there will be a delay of several days before you can pick it up.
- Have showers rather than baths. Place a handle on the shower wall and a footstool outside and inside to help you in and out.
- You may drive a car.
- Please return to see me four months AFTER SURGERY (approximately 2 and a half months from now) for an examination of your operated knee.
- Long term care: You should have periodic examinations and x-rays of your knee replacement. I will discuss with you the frequency of such visits based on your age and activity level. Follow us on Facebook, Twitter and Instagram (@NYHipKnee ) for periodic updates on conditions that may affect your knee replacement as well as updates on how to make it last longer.
For additional information, instructions and educational videos please visit www.agdvmd.com
Prevention of traveler’s thrombosis
During the first 3 months after a total joint replacement, you are at an increased risk of developing clots in the veins of your legs and thighs (deep venous thrombosis). Clots in the legs are not serious, but occasionally they break off and travel to the lungs (called pulmonary embolism) causing chest pain and shortness of breath. This is not a common occurrence, but when it does happen, it can be life threatening.
One of the causes of clot formation is prolonged immobilization, such as sitting for many hours at a time. Prolonged immobilization can occur in an airplane, car, train, or bus.
Although healthy individuals may develop clots, those with underlying risk factors such as cancer, obesity, varicose veins, coronary artery disease, certain blood diseases, a history of blood clot formation, pregnancy, women taking oral contraceptive pills, or those on estrogen replacement therapy, are at a higher risk.
In order to minimize the risk of traveler’s thrombosis, the following is recommended for all travelers:
- Do not place baggage underneath the seat in front of you because that reduces the ability to move the legs.
- Wear elastic stockings and loose-fitting clothing.
- Avoid crossing your legs at your ankles or knees.
- Regularly change leg position and exercise the legs by flexing and extending the ankles at regular intervals while seated.
- Walk about the cabin periodically and when flight conditions permit.
- Do not sleep in a cramped position and avoid the use of sleep aids.
- Drink adequate amounts of water, milk and fruit juices to maintain good hydration. Avoid or minimize dehydrating drinks such as alcohol or caffeinated beverages.
If there are risk factors as mentioned above, additional preventive measures may be considered for you, including taking a baby aspirin one hour before traveling or an anticoagulant (blood thinner) medication. I will gladly discuss your particular situation during your office visit.
For additional information, instructions and educational videos please visit www.agdvmd.com
Hip replacement precautions
The recovery of your hip is now well advanced. From now on, you can reduce the daily exercises to about once or twice a week. You can basically lead a normal life.
However, remember that your hip is an artificial device, even if it feels “normal”. As with any artificial device, there is a risk of mechanical failure. Thus, I would recommend that you follow these precautions for the rest of your life:
IF POSSIBLE AVOID THE FOLLOWING:
- Being overweight. If you are, make every effort to lose weight. The lighter you are the longer your hip will last. For additional information, please ask me or my office staff.
- Lifting and carrying weights over approximately 30-40 pounds.
- Jumping, running or causing any significant repetitive impact on your hip.
- Stairs: use a banister.
- Strenuous sports, particularly contact sports. However, you may swim, do water exercises, use a stationary or regular bicycle, treadmill, or Nordic track, in a gentle fashion. You can play golf using a cart and gentle double tennis, preferably on a soft court. For more information regarding activity following total joint replacement, please ask me or my office staff.
If you develop an infection anywhere in your body, contact your doctor. Infections should be treated adequately and promptly. There is a remote chance of the infection seeding the artificial hip through the blood stream. For the same reason, if dental work, or other surgery is to be performed, we recommend prophylactic antibiotics. Inform your dentist and doctors that you have a total hip replacement.
The periodic examination of your hip replacement is paramount. You should have periodic examinations and X-rays of your joint replacement. I will discuss with you the frequency of such visits based on your age and activity level. The mechanical failure of a total hip replacement is initially a silent process. If detected early, through periodic radiographic examinations, several treatments can be instituted before you start having pain and severe loss of bone occurs.
Follow us on Facebook, Twitter and Instagram (@NYHipKnee) for periodic updates on conditions that may affect your joint replacement as well as updates on how to stay healthy and make your implant last longer.
If you move, please contact our office and inform my secretary of your new address and telephone number in case we need to contact you in the future.
Knee replacement precautions
The recovery of your knee is now well advanced. Knee strengthening exercises can be performed only if needed. You can basically lead a normal life.
However, remember that your knee is an artificial device, even if it feels “normal”. As with any artificial device, there is a risk of mechanical failure. Therefore, in order to increase the longevity of your knee replacement, I would recommend that you follow these precautions for the rest of your life:
IF POSSIBLE AVOID THE FOLLOWING:
- Being overweight. If you are, make every effort to lose weight. The lighter you are the longer your knee will last. For additional information, please ask me or my office staff.
- Lifting and carrying weights over approximately 30-40 pounds.
- Jumping, running or causing any significant repetitive impact on your knee.
- Walking over four to five miles a day. Wear well-padded shoes with rubber soles and heels. It is preferable to walk on soft terrain rather than hard concrete.
- Stairs: Use a banister.
- Strenuous sports, particularly contact sports. However, you may swim, do water exercises, use a stationary bicycle, treadmill or Nordic track in a slow, gentle fashion. You can play golf using a cart and gentle double tennis, preferably on a soft court. For more information regarding activity following total joint replacement, please ask me or my office staff.
If you develop an infection anywhere in your body, contact your doctor. Infections should be treated adequately and promptly. There is a remote chance of the infection seeding the artificial knee through the blood stream. For the same reason, if dental work, or other surgery is to be performed, we recommend prophylactic antibiotics. Inform your dentist and doctors that you have a total knee replacement.
The periodic examination of your knee replacement is paramount. You should have periodic examinations and X-rays of your joint replacement. I will discuss with you the frequency of such visits based on your age and activity level. The mechanical failure of a knee replacement is initially a silent process. If detected early, through periodic radiographic examinations, several treatments can be instituted before you start having pain and severe loss of bone occurs.
Follow us on Facebook, Twitter and Instagram (@NYHipKnee) for periodic updates on conditions that may affect your joint replacement as well as updates on how to stay healthy and make your implant last longer.
If you move, please contact our office and inform my secretary of your new address and telephone number in case we need to contact you in the future.
Physical activity / sports following total joint replacement
After surgery, your hip and/or knee replacement will wear at a slow pace. The heavier, younger and more active you are, the faster the wear process will be. Excessive wear of your arthroplasty is initially a silent problem (will cause no pain), but in the long term, it will result in loss of bone around your joint (osteolysis). Osteolysis can eventually lead to the failure of your prosthesis which may then need to be re-operated. Enclosed please find the activities that you can safely do, those which you can do if you have experience, and those you should avoid.
Please remember that the recommended physical activities should be performed in moderation.
Allowed: Walking, hiking, trekking, swimming, water-polo, water aerobics, low impact aerobics, road bicycling, stationary bike, golf, croquet, shuffleboard, bowling, dancing, horse shoes, shooting, fishing, sailing.
Allowed with experience: Jazz dancing, square dancing, fencing, stationary cross-country skiing, cross-country skiing, downhill skiing, intermediate slopes (no moguls), ice skating, roller/inline skating, light weight lifting (sitting or lying down), light weight machines, tennis (on soft court, social, not competitive, doubles).
Not recommended: High impact aerobics, baseball/softball, basketball, football, lacrosse, soccer, gymnastics, handball, hockey, volleyball, running, competitive tennis, racquetball, squash, rock climbing, and horseback riding.
Please, use your judgment to adapt to the physical activity according to your age, general physical condition and experience. If in doubt, be cautious and protective of your joint replacement.
Long term care: You should have periodic examinations and X-rays of your joint replacement. I will discuss with you the frequency of such visits based on your age and activity level. Follow us on Facebook, Twitter and Instagram (@NYHipKnee) for periodic updates on conditions that may affect your joint replacement as well as updates on how to stay healthy and make your implant last longer.
For additional information, instructions and educational videos please visit www.agdvmd.com
Antibiotic prophylaxis instructions
Your total joint replacement is at a low risk of becoming infected by bacteria traveling through your bloodstream. This risk can be lowered by promptly treating any infection in your body, particularly those in your gums and teeth, skin, ears, kidneys and bladder, intestines, lungs, and heart.
The most critical period is the first two years after joint placement. If you develop sudden pain in your prosthetic joint during the course of a bacterial infection you should seek medical attention promptly.
During the first two postoperative years, you should receive antibiotic prophylaxis before dental procedures that involve substantial bleeding like dental extractions, root canal, dental implant placement, teeth cleaning, among others. You may also need antibiotics before some urological procedures, or during the course of other conditions such as recent or recurrent urinary tract infection, or recent / recurrent prostatitis.
Suggested antibiotic prophylaxis regimen for dental procedures
- Patients not allergic to penicillin: cephalexin, cephradine or amoxicillin: 2 grams orally 1 hour prior to dental procedure.
- Patients not allergic to penicillin and unable to take oral medications: cefazolin 1 gram or ampicillin 2 grams intramuscularly or intravenously 1 hour prior to the procedure.
- Patients allergic to penicillin: clindamycin: 600 mg orally 1 hour prior to the dental procedure.
- Patients allergic to penicillin and unable to take oral medications: clindamycin 600 mg intravenously, 1 hour prior to the procedure.
Suggested antibiotic prophylaxis regimen for urological procedures
- A single systemic level dose of a quinolone (e.g., ciprofloxacin, 500 mg; levofloxacin, 500 mg; ofloxacin, 400 mg) orally one to two hours preoperatively.
- Ampicillin 2 gm IV (or vancomycin 1 gm IV over 1 to 2 hours, in patients allergic to ampicillin) plus gentamicin 1.5 mg/kg IV 30 to 60 minutes preoperatively.
You don’t need antibiotic prophylaxis before receiving a manicure, pedicure, gynecologic routine examination, injection, or eye surgery.
Long term care: You should have periodic examinations and X-rays of your joint replacement. I will discuss with you the frequency of such visits based on your age and activity level. Follow us on Facebook, Twitter and Instagram (@NYHipKnee) for periodic updates on conditions that may affect your joint replacement, updates on how to stay healthy and make your implant last longer.
Safety tips to prevent falls
Falls can cause serious injuries and as we age, the risk of falling increases. If you have already fallen, you have a higher risk of having a future fall. I would recommend that you follow the next recommendations to prevent new falls:
Check with your family doctor / internist to rule out medical conditions that may explain the falls and to assure that the medications you may be taking do not affect your balance and increase the risk of falls.
Check your vision and update your glasses prescription. Do not walk with reading glasses.
When entering a room, make sure the lighting is appropriate and look for thresholds, obstructing objects and uneven floor surfaces. All the rooms where you live should have adequate lighting.
Keep all floor surfaces smooth, free from tripping hazards such as cords, wires and unexpected objects. Be disciplined in the storage of shoes and other articles, making sure they do not obstruct the usual pathways and arrange furniture to allow easy ambulation.
Wear supportive, low heel shoes. Do not walk in slippery socks. Avoid slippery and wet floor surfaces. The carpets should be tacked to the floor without protruding edges. Rugs should have anti-skid backing and the edges should not fold. It may be even safer to remove the rugs. Stairs should be well lit and with adequate rails. Hold onto rails when going up and down the stairs, particularly if you are carrying things that obstruct your view, i.e. laundry.
Install grab bars in the shower, bathtubs and toilets. Place an anti-skid rubber bathmat in the shower and tub. Wet surfaces are particularly slippery.
If your balance is poor, take shorter steps and use a cane for ambulation outdoors with a proper rubber tip. Four pronged canes provide even more support. Indoors you can lean on furniture for extra balance. When you wake-up, sit on the edge of the bed and make sure you are not dizzy before you stand.
Outdoors: avoid ice, sleet and snow. If you use public transportation, make sure you hold onto the grab bars. Do not walk while the vehicle is in motion. Do not hesitate to request a seat if necessary. Take your time getting in and out.
Make sure you can reach a telephone to call for help if you fall. Consider carrying a portable phone, or getting a personal emergency response system (PERS), especially for older patients who live alone. A PERS can prevent lengthy “lie-time” in the event of a fall and may increase feelings of security and confidence.
If despite all these measures you still feel insecure, ask for assistance from a relative or friend. If you live alone, you may consider moving to an assisted-living facility.
For additional information, instructions and educational videos please visit www.agdvmd.com
Instructions to prevent hip replacement dislocations
Dislocation is a rare event after a total hip replacement. It means that your prosthetic ball came completely out of the socket. In most cases, gentle traction of your leg with mild sedation allows relocation of the prosthesis. Surgery is seldom necessary to reduce a dislocated hip.
Though the risk of dislocation is low after the third postoperative month, dislocation can occur late, years or decades after your operation. The dislocation can be produced by multiple factors, including trauma due to a fall or accident, failure to avoid the positions that can dislocate your hip, poor muscle tension across your hip, among others. Some patients may experience a partial, painful dislocation (subluxation) if they do not comply with the hip precautions.
Once your hip dislocated, there is damage of the soft tissue envelope around your hip and the likelihood of having a new dislocation is higher than if you would have never dislocated your hip. Therefore, prevention is paramount.
- In order to prevent a dislocation, please follow the following instructions:
- Sit in high armchairs and use a high toilet seat (approx. 24 inches high).
- Raise your bed to about 24 inches by placing an extra mattress or blocks under its feet.
- Do not bend the hip more than 90 degrees.
- Do not cross your knees.
- When in bed, keep a pillow between your knees.
- To reach your foot, bring your knee outwards and the foot inwards, so that you see the inner part of your thigh, knee and leg. If you cannot reach your foot easily, do not force it (See over).
- If you have to pick up objects from the floor, lean on a piece of furniture and do it as shown (See over).
- Do the exercises shown in the back of this sheet to strengthen the muscles of your hip. Start doing them standing, slowly, gently, a few minutes in the morning and in the evening. The exercises should not hurt. Increase the number of repetitions as tolerated. Once they become easy, you can also do them lying down in bed (as shown), which demands a greater effort.

Instructions to prevent limited range of motion after knee replacement
Stiffness can rarely develop following a knee replacement. This means that the mobility of your knee is not enough to perform regular activities like walking, negotiating stairs, sitting down, standing up, or reaching your foot comfortably. You can have difficulty straightening your knee (loss of extension), bending your knee (loss of flexion), or both. In addition, stiffness can be painful.
The early healing process following surgery involves the formation of scar tissue around the knee replacement parts. The formation of a regular amount of loose scar tissue is normal. However, a few patients can develop a thick, fibrous scar that can limit mobility of your knee (arthrofibrosis). The development of arthrofibrosis depends on multiple factors and can be exacerbated by insufficient exercising of your knee after surgery.
The period in which you can gain range of motion following surgery is limited. During the first 3 to 4 months you will gain most of the mobility in your new knee. Therefore, it is paramount that you exercise conscientiously and enthusiastically now, to achieve the best possible result. For patients who develop stiffness after this early period, the treatment is more difficult and less effective.
At this point, the mobility of your knee is limited as I discussed during your visit. I would recommend that you follow my physical therapy instructions and that you exercise consistently while you are at home.
Adequate pain control is important for you to exercise comfortably and re-gain the mobility of your stiff knee. Pain control can be obtained by the use of the prescribed pain medication and by frequently icing the knee. I recommend that you take pain medication one hour before physical therapy and after that as needed according to my instructions.
Please follow these instructions during the next weeks:
- Avoid keeping your knee bent while you are in bed: Do not place a pillow under your knee, and avoid resting with your knee on the side. Keep your feet pointing up. A knee that is slightly bent will hurt less but will heal bent.


- The following exercises will increase the flexion and extension of your knee. Practice several repetitions at home and with your physical therapist. Some pain is expected and does not mean that you are damaging your operation. You are stretching and breaking the bands of thick scar tissue that are forming in your knee.

I would like to learn about your progress. Please, call me and have your physical therapist call me in two weeks. I would like to learn about your progress and the range of motion that you achieved after following these instructions (please ask your physical therapist to measure the range of motion of your knee with a goniometer). If the range of motion is not acceptable, you may require a manipulation of your knee replacement under anesthesia (breaking the scar tissue by gently manipulating your knee while you are under anesthesia).
Back care
- Do the prescribed exercises when your pain has subsided to prevent further back problems.
- Do use a heating pad intermittently on your back area.
- Do sleep on a firm mattress and sit on a slightly higher chair, preferably with armrest. To get out of the bed, lay on your side on the border of the bed so that your legs dangle, and then, sit up on your side. Do the reverse movement to lay down on the bed.
- Do use your hands to assist yourself from rising or settling into a high chair, for holding onto a rail on stairs, and to assist yourself in bending to pick up something.
- Do stoop with your knees and not your back.
- Do gentle, non-impact sports like swimming or stationary bicycle.
- Do take your medication as prescribed by your physician.
Don’ts
- Don’t do any exercises when your back is in acute pain. Be very cautious about doing other than prescribed exercises. Avoid sit-ups and bending exercises.
- Don’t sit in one position for more than half hour; rather alternate sitting with standing. Avoid soft, low seats.
- Don’t drive a car when your back is in acute pain. Use a wire wicker type of back seat support.
- Don’t stand in a partially bent position for any length of time, i.e., gardening.
- Don’t smoke.
EXERCISES





